SPECIAL COVERAGE
Read More
Read More
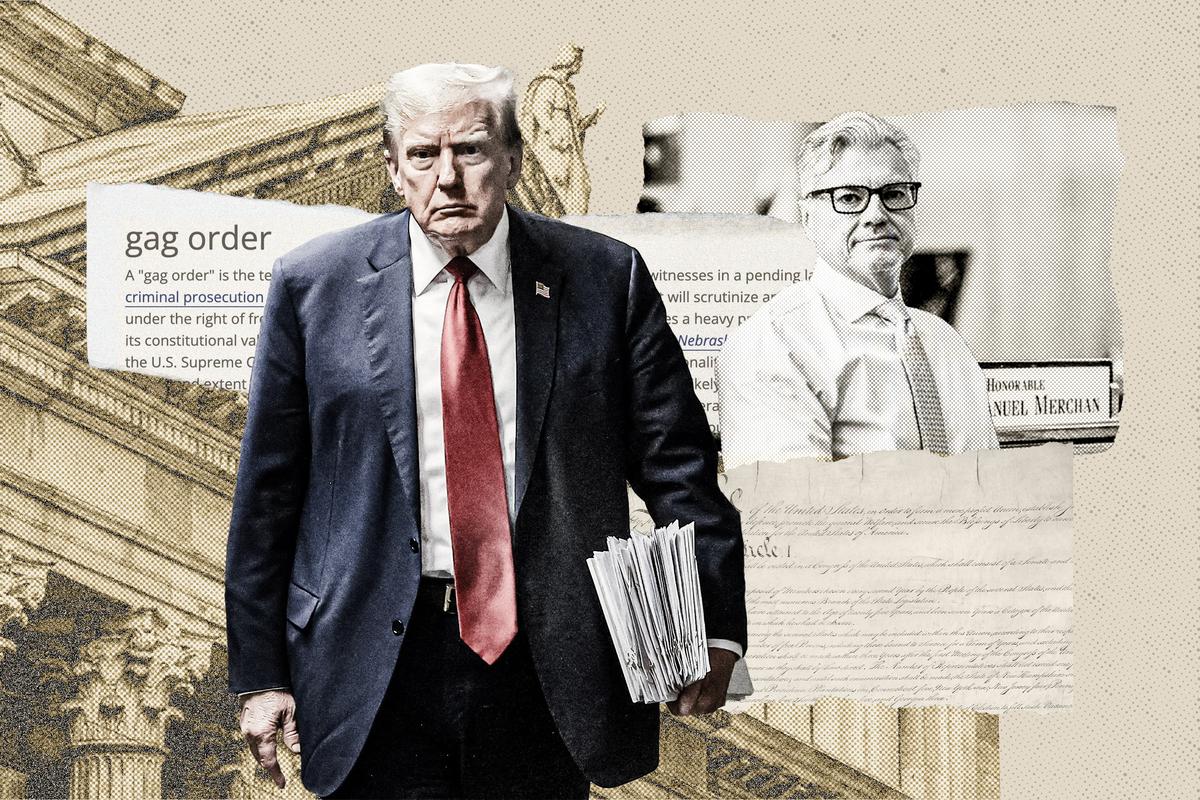
Special Counsel Jack Smith Admits Prosecutors Misled Judge in Trump Case
Prosecutors say they’re not sure what happened.
Special Counsel Jack Smith Admits Prosecutors Misled Judge in Trump Case
Prosecutors say they’re not sure what happened.
Trending Videos
Top Premium Reads
Top Stories
Most Read
The Firing Squad: A Film That Just Might Change America
‘I believe we will save and change America.’
DHS Shuts Down Expert Group That Denied Hunter Biden Laptop Story
A conservative nonprofit filed a lawsuit claiming extreme political bias, following which, the federal agency disbanded the bunch of political advisors.
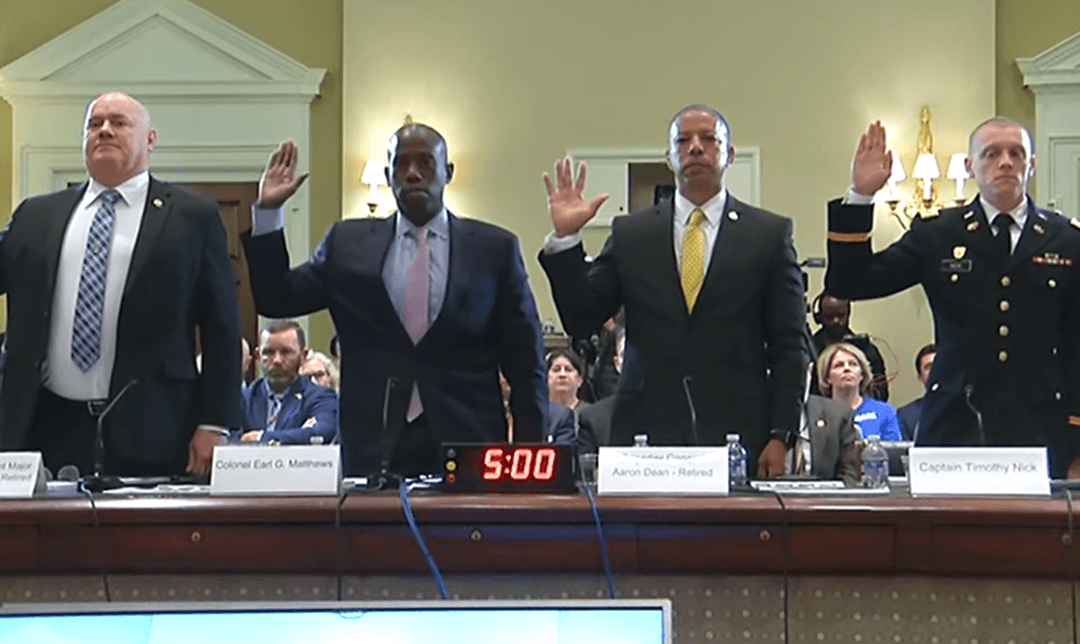
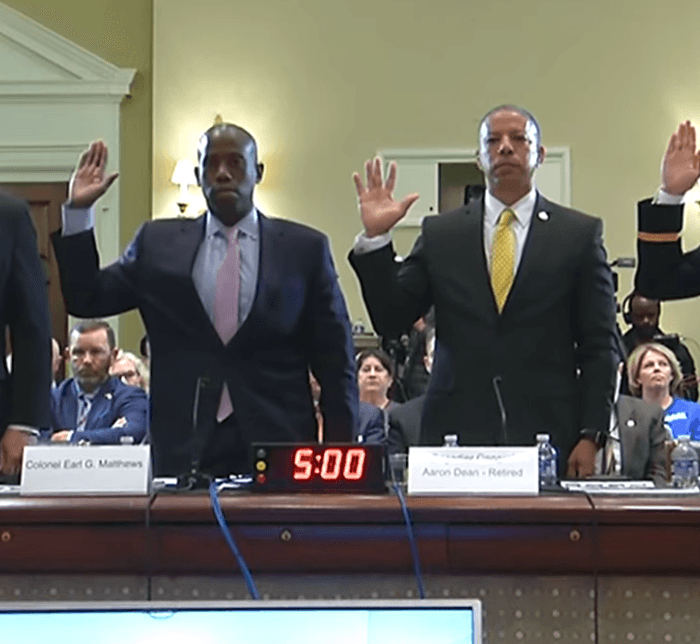
Military Leaders Plotted to Disobey Trump’s Orders as Commander-in-Chief on Jan. 6, Whistleblower Claims
Maj. Gen. Walker conveyed a request for assistance at around 1:50 p.m. on Jan. 6 but the Guard was not deployed to the Capitol until about 5:10 p.m.
Biden DOJ Official Admits to Misleading Congress on Her Arrest Record
Kristen Clarke claims to be a victim of domestic violence and argues that she was obligated to disclose that information.
Japan Refutes Biden’s Comments Describing the Country as ‘Xenophobic’
President Joe Biden said that Japan, along with three other countries, was struggling economically due to its refusal to accept immigrants.
Biden Administration Finalizes Rule to Allow ‘Dreamers’ to Enroll in ’Obamacare’
The new directive is expected to provide coverage to approximately 100,000 immigrants next year.
Economist Shoots Down White House Shrinkflation Claims
Other economists assert corporate greed is lifting inflation pressures.
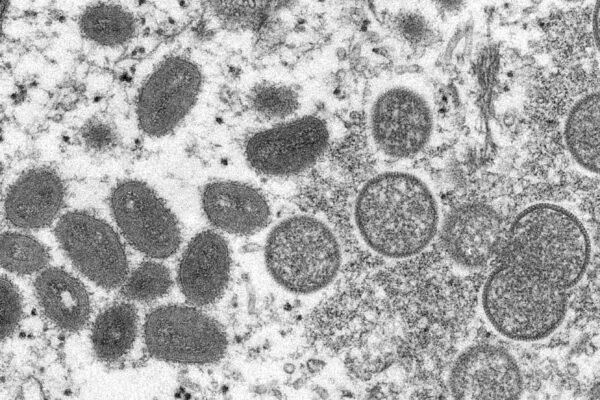
Terrain Theory vs. Germ Theory–A Fresh Look at an Old Principle
The theory that a strong and healthy body keeps illness at bay is reemerging as a foundation for maintaining wellness and fighting potential disease.
Iowa Defiant as DOJ Threatens Lawsuit to Block Illegal Immigrant Law: ‘Will Not Back Down’
‘I have a duty to protect the citizens of Iowa. Unlike the federal government, we will respect the rule of law and enforce it,’ Iowa governor said.
House Panel Calls to Defund Federal Agencies That Stonewall Congressional Probes
Biden administration accused of defying congressional authority by being reluctant to comply with legitimate oversight requests.
Amid Closer Ties With China, Russia Raids Homes of Falun Gong Practitioners
‘We are concerned about this whether it happens in China or Russia or elsewhere in the world,' a White House National Security Council spokesperson said.
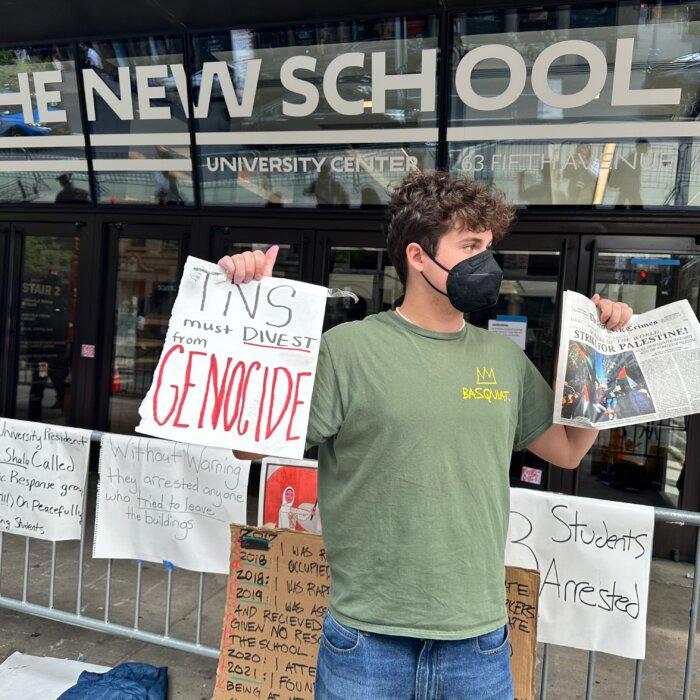
White House Commends ‘Admirable’ Students Protecting American Flag
White House press secretary Karine Jean-Pierre says deploying the National Guard ‘is something that governors decide on.’
Sen. Manchin Slams Final EV Tax Credit Rules: Endorsing ‘Made in China’
Mr. Manchin considers the final eased rules as ‘providing a long-term pathway’ for China and other foreign adversaries to ’remain in our supply chains.’
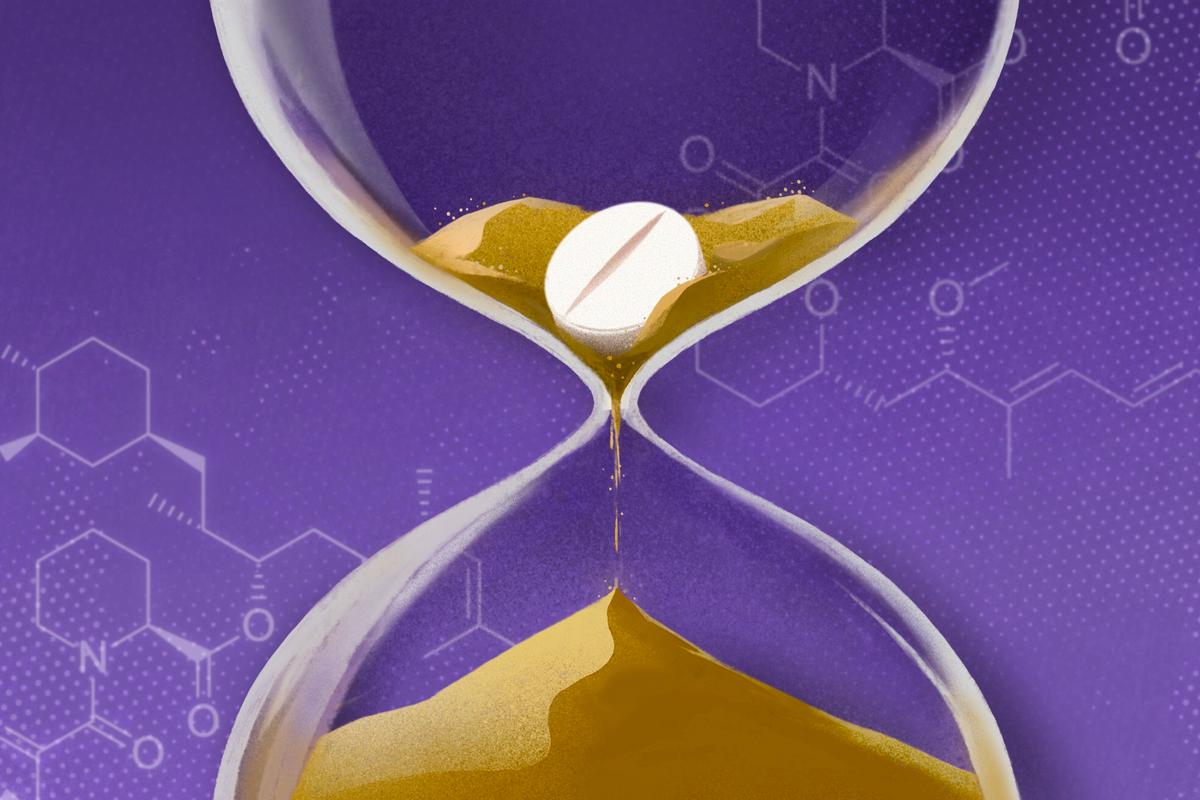
Lipid Nanoparticles Cause Inflammation in Cells, but Damage Can Be Reduced: UPenn Preprint
The study found that lipid nanoparticles cause inflammation by damaging cellular components called endosomes, but the degree of inflammation varies.

24 Hours in Istanbul
Straddling Europe and Asia, Turkey’s largest city beckons with fascinating history, colorful bazaars, and excellent food.
24 Hours in Istanbul
Straddling Europe and Asia, Turkey’s largest city beckons with fascinating history, colorful bazaars, and excellent food.
Epoch Readers’ Stories
A History Of The American Nation
A patriotic poem by Ted Schneider
Of Cars and Kids
Why should our kids have to settle for a Trabant, or a Pyonghwa, education when they could have a BMW?
A Nation Divided
Poem by an American Patriot
What Is Going on Here?
There are two major things plants need to survive and continue generating our life saving oxygen. The first is CO2, and the second is sunshine.
Inspired Stories
Empower the World with Your Story: Share Love, Inspiration, and Hope with Millions
Special Coverage
Special Coverage

Lower Mortality With Fewer Than 10,000 Steps a Day
You don’t need to have a fancy gym membership to land the benefits derived from walking.

Lower Mortality With Fewer Than 10,000 Steps a Day
You don’t need to have a fancy gym membership to land the benefits derived from walking.

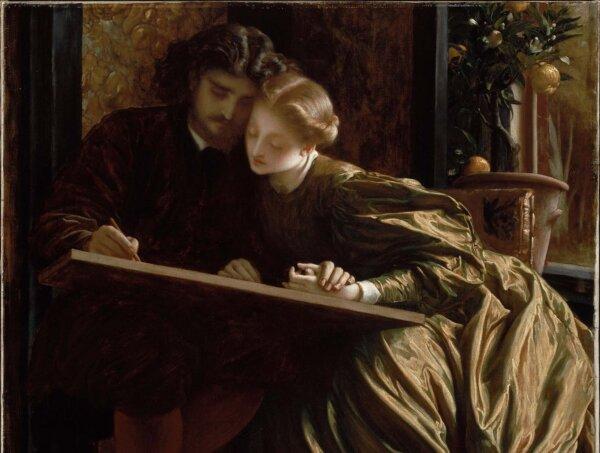
Raphael’s ‘Sistine Madonna’
Famous for his paintings of the Virgin, Raphael’s composition is admired for its extraordinary juxtaposition of a celestial vision and the earthly realm.

‘The Idea of You': Anne Hathaway Will Steal Your Heart. Again.
Filmmaker Michael Showalter delivers another unexpected, genre-defying gem.
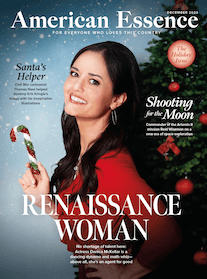
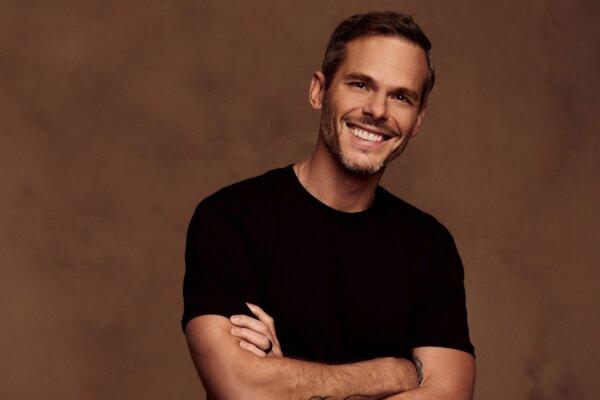
From Country Music to Ministry: Granger Smith Shares the Faith Journey That Set Him on a Path Beyond Music
Through faith, Granger Smith was able to overcome the unimaginable grief at his son’s death. Now he’s set on a path to help others process their loss.

Railroad Magnate and Governor Mansion
The Leland Stanford Mansion is a stunning example of Victorian era splendor in the heart of Sacramento.
‘Second Class’: The Working Class Struggles
Author Batya Ungar-Sargon believes there is a growing class divide between service and knowledge workers.

Greek Burgers With Feta Aioli
These insanely flavorful Greek Burgers have seasoned turkey patties topped with feta aioli, grilled onions and arugula.

Unusual Tours Teach Local Culture With Flair
There are areas around the country where people go to experience unusual phenomenon.

Taking the Kids: And Shopping Smarter (And More Sustainably) for Mother’s Day
Treat mom to gifts that also give back to the environment.

Traveling This Year? Here’s What You Need to Know About TSA PreCheck, CLEAR Plus and Global Entry
While each offer similar privileges, the three programs often get conflated together.
Unusual Tours Teach Local Culture With Flair
There are areas around the country where people go to experience unusual phenomenon.






























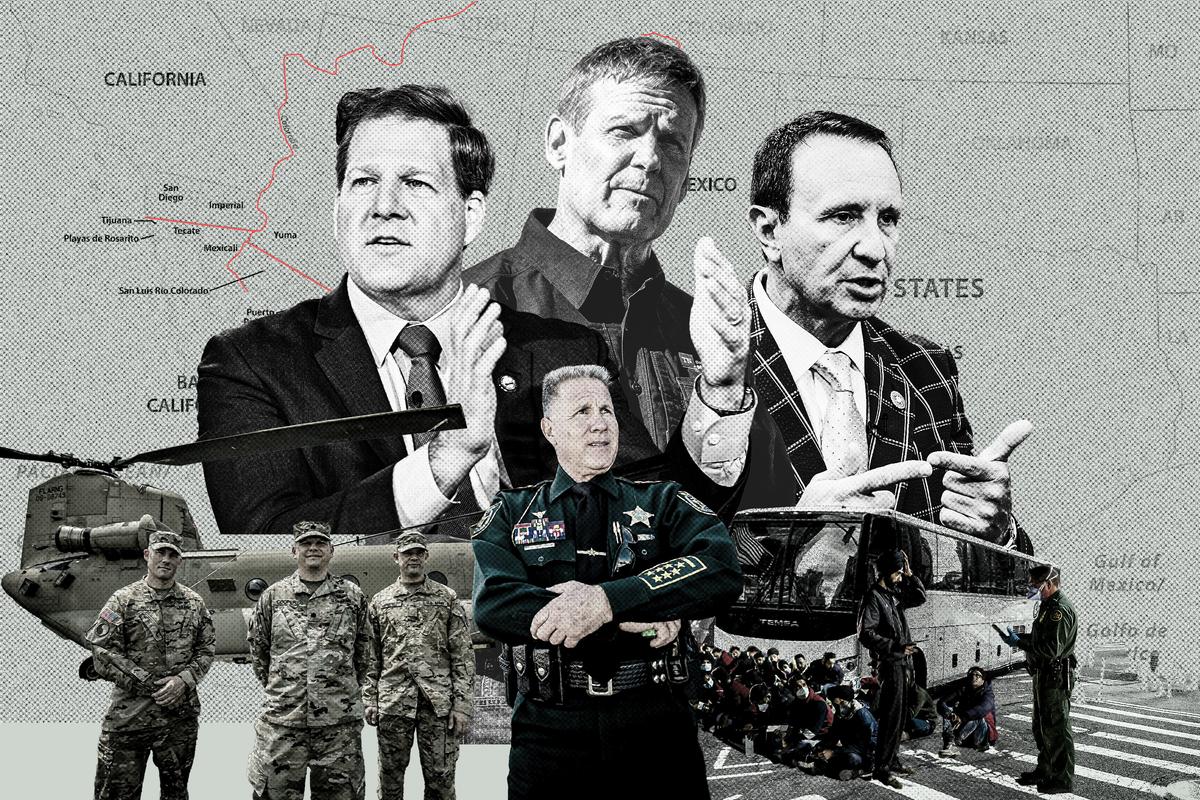







![[PREMIERING MAY 9, 8:30PM ET] Weapons of Mass Migration | NEW Documentary](/_next/image?url=https%3A%2F%2Fimg.theepochtimes.com%2Fassets%2Fuploads%2F2024%2F05%2F04%2Fid5643663-900x1350-600x900.jpg&w=1200&q=75)




























































![[PREMIERING 5/4, 9PM ET] RFK Jr. Takes on Trump and Biden Over Four ‘Existential’ Issues](/_next/image?url=https%3A%2F%2Fimg.theepochtimes.com%2Fassets%2Fuploads%2F2024%2F05%2F04%2Fid5643727-240501-ATL_RFK_HD_TN-600x338.jpg&w=1200&q=75)