SPECIAL COVERAGE
Read More
Read More
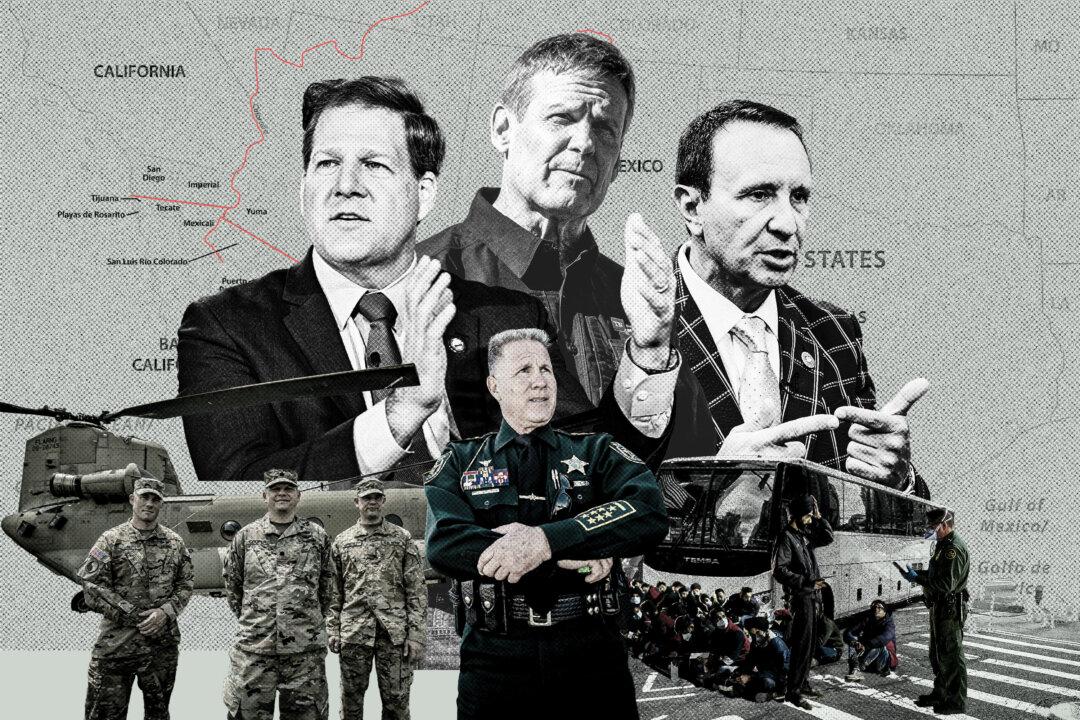
These States Are Making It Illegal for Illegal Immigrants to Enter
Thousands of miles from the border, red states are taking matters into their own hands as the border crisis persists.
These States Are Making It Illegal for Illegal Immigrants to Enter
Thousands of miles from the border, red states are taking matters into their own hands as the border crisis persists.
Top Premium Reads
Top Stories
Most Read
A Peaceful Appeal for Freedom 25 Years Ago Still Echoes Today
About 10,000 people congregated in Beijing on a spring day in 1999, in the largest protest in China’s recent history—known as the April 25 appeal.
Supreme Court Seems Open to Allowing Some Presidential Immunity, May Delay Trump Trial
Justices wrestled with how to define a president’s ‘official’ versus ‘private’ acts. A decision may delay President Trump’s trial, which would hand him a win.
Fed’s Preferred Inflation Gauge Tops Estimates as Price Stability Progress Stall
Next inflation stop will be the consumer price index.
Congressional Commission Demands CCP End Decades-Long Persecution of Falun Gong
Less than three months after the appeal, on July 20, 1999, the Chinese Communist Party launched the brutal persecution of Falun Gong adherents across China.
Planes Almost Collide at 2 Major Airports as Boeing Probe Advances
Some aviation experts argue the FAA’s focus on ‘diversity’ instead of ’merit' in hiring pilots and controllers is leading to serious safety concerns.
Southwest Pulling out of 4 Airports Due to First Quarter Loss, Boeing Problems
The loss was worse than expected.
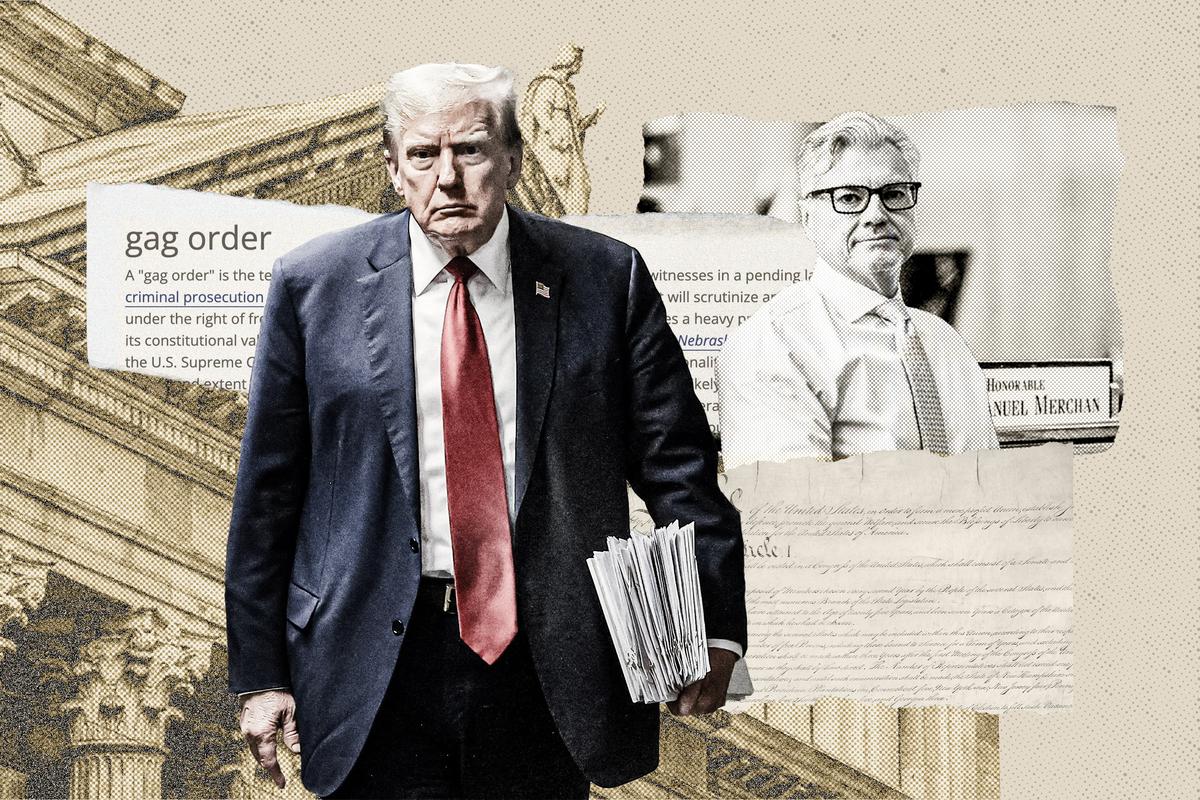
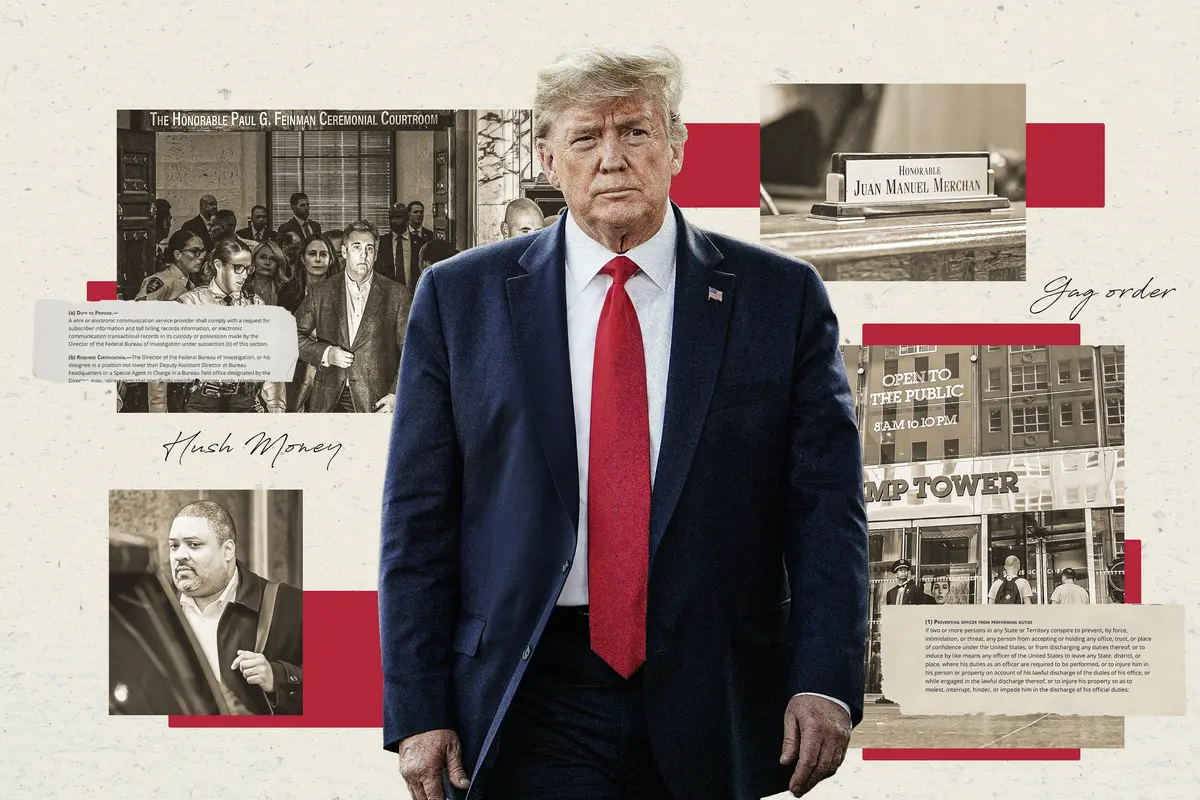
Manhattan DA Accused of Politically Motivated Prosecution in Trump Trial: House Report
‘Bragg’s politically motivated prosecution of President Trump threatens to destroy this notion of blind justice,’ the committee alleges.
Pentagon Moving Ahead With Plans to Pull US Troops From Niger, Draw Down in Chad
While working to expel Western forces that have previously been stationed in the country, Niger’s junta government has begun to form partnerships with Russia.
Key Takeaways From Trump’s Supreme Court Immunity Appeal
A Trump attorney argued that presidents will be hamstrung in office and open to extortion if they are not guaranteed immunity for official acts.
FCC Reinstates Net Neutrality Rule, Upending Trump-Era Decision
The net neutrality rules were first implemented by the FCC under Obama, but the commission reversed course during President Donald Trump’s administration
Indo-Pacific Spending Bill Puts $8 Billion Toward Countering Communist China
‘It’s no secret Communist China is eyeing an invasion of Taiwan, and [Chinese leader] Xi is watching the United States closely,’ said Rep. Bob Latta.
Editors' Picks
Judge Unseals Documents Showing FBI Discussed ‘Loose Surveillance’ of Trump’s Plane
A large tranche of documents were unsealed by Judge Aileen Cannon on Monday, revealing the FBI’s code name for the probe.
Certain Teas May Inactivate COVID-19 Virus, Lab Study Finds
But experts caution against overstating potential real-world benefits.
Biden Awards Micron $6 Billion to Boost Chip Production in US
President Biden hailed the investment during a speech in Syracuse, New York, calling it “a big deal.”
JPMorgan CEO Issues Dire Warning About Biden Admininistration’s ‘Huge’ Deficit Spending
‘Deficits which basically aren’t going to go away as far as the eye can see,’ JPMorgan CEO Jamie Dimon said, while warning of stagflation.

Mahler’s ‘Resurrection’ Symphony: Answering Nihilism
Mahler’s “Resurrection” Symphony is the musical equivalent of “Hamlet.” What led to its creation?
Mahler’s ‘Resurrection’ Symphony: Answering Nihilism
Mahler’s “Resurrection” Symphony is the musical equivalent of “Hamlet.” What led to its creation?
Epoch Readers’ Stories
A History Of The American Nation
A patriotic poem by Ted Schneider
Of Cars and Kids
Why should our kids have to settle for a Trabant, or a Pyonghwa, education when they could have a BMW?
A Nation Divided
Poem by an American Patriot
What Is Going on Here?
There are two major things plants need to survive and continue generating our life saving oxygen. The first is CO2, and the second is sunshine.
Inspired Stories
Empower the World with Your Story: Share Love, Inspiration, and Hope with Millions
Special Coverage
Special Coverage

Starting Antihypertensive Medications Associated With Higher Risk of Falls, Fractures
When first initiated, blood pressure-lowering drugs pose an increased risk of falls for residents living in health care facilities, a new study shows.

Starting Antihypertensive Medications Associated With Higher Risk of Falls, Fractures
When first initiated, blood pressure-lowering drugs pose an increased risk of falls for residents living in health care facilities, a new study shows.
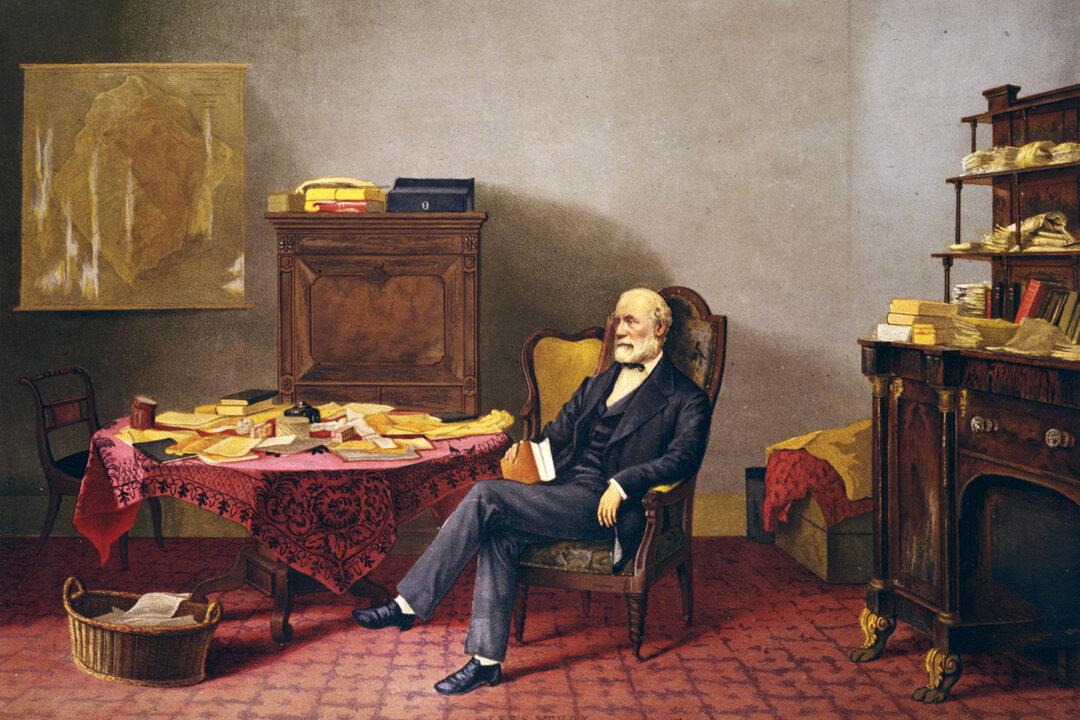
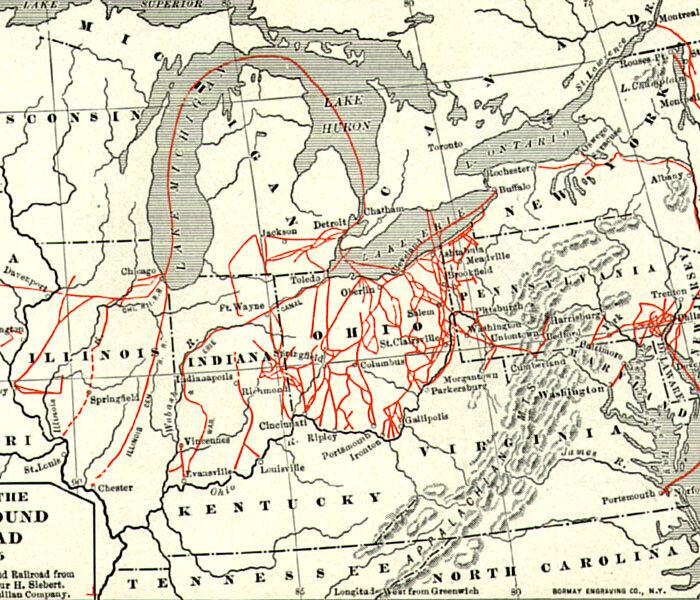
The Two Reputations of Robert E. Lee
While those in the past saw Lee’s stellar qualities, today, some cannot see that he was a man defined, like all of us, by his time.
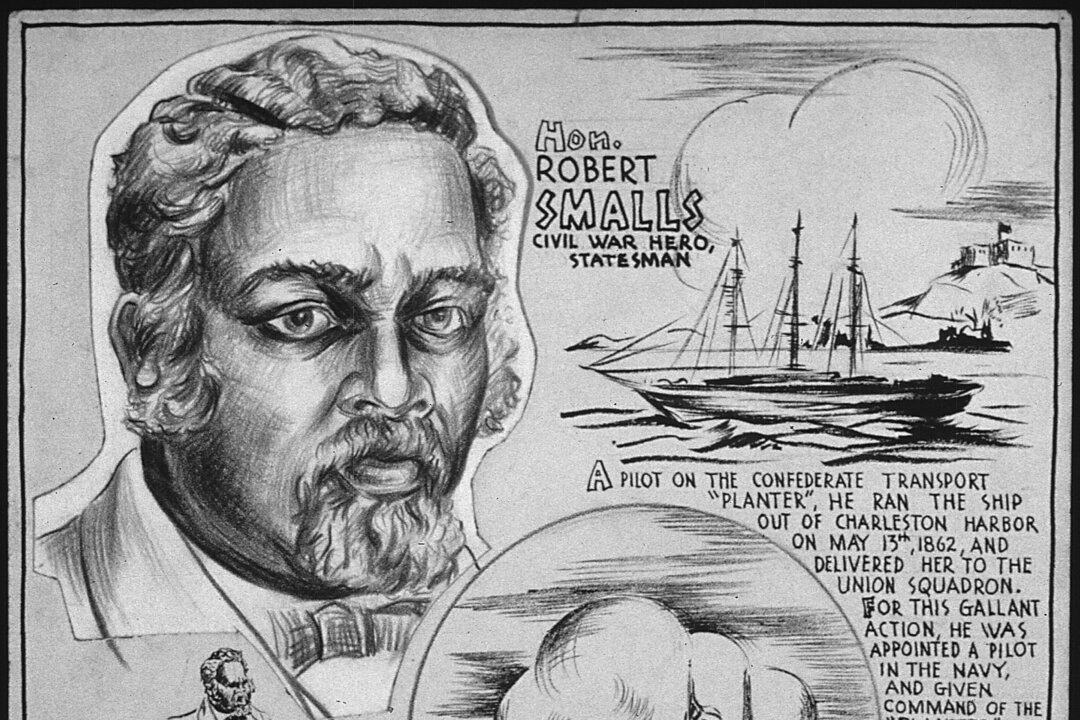
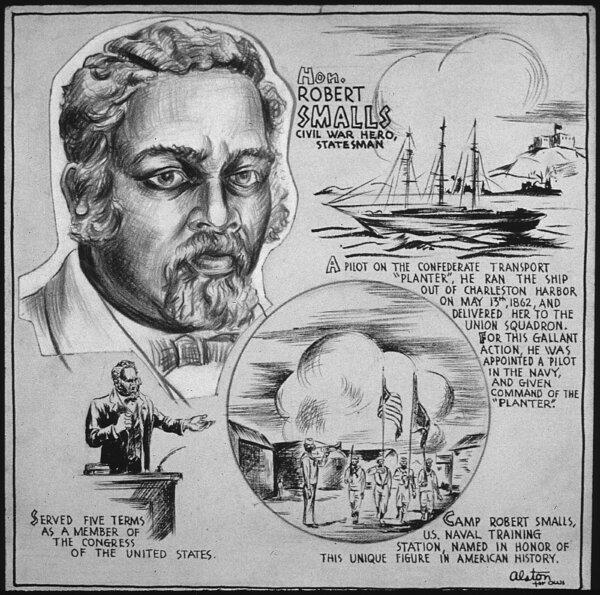
Robert Smalls: Navy Captain and Reconstruction-Era Politician
This former slave would not let anything stop him on the road to freedom.

Spotlight on Supplements: Kava
Kava is reported to be beneficial to stress and anxiety but its comes with side effects.

Taking the Kids: To the Smithsonian Museums
The Smithsonian Institution is the world’s largest museum, education and research complex.

Airbnb Rentals Could Be Harder to Come by in Hawaii. Here’s Why and When That Might Happen
New bills will give counties the power to limit short-term rentals amidst housing shortages.

These Texas Airports Have Flight Cancellation Rates That Place Them Among the Highest in the Country, Study Finds
Airports across the country have made the list with New York and New Jersery placing in the top 3.
Taking the Kids: To the Smithsonian Museums
The Smithsonian Institution is the world’s largest museum, education and research complex.





























































































































![[LIVE 4/26 at 10:30AM ET] New Push Started for Global Digital Currencies](/_next/image?url=https%3A%2F%2Fimg.theepochtimes.com%2Fassets%2Fuploads%2F2024%2F04%2F19%2Fid5633115-0426-600x338.jpg&w=1200&q=75)