About 34 million people in this country alone have low bone density and many over 60 have osteoporosis. But don’t expect bisphosphonate meds to strengthen your bones. Instead, they may raise your risk for fracture. Plus, most load-bearing exercises don’t provide enough of a load to help.

Javier Regueiro/Shutterstock
|Updated:
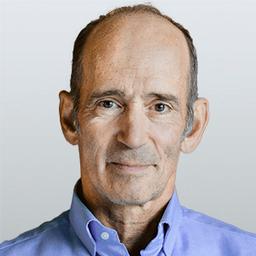
Dr. Joseph Mercola is the founder of Mercola.com. An osteopathic physician, best-selling author, and recipient of multiple awards in the field of natural health, his primary vision is to change the modern health paradigm by providing people with a valuable resource to help them take control of their health.
Author’s Selected Articles