Since the start of the pandemic, natural supplements have been a bone of contention with researchers, pharmaceutical companies, doctors and health experts. Newly published data again support past research that vitamin D has a significant impact on COVID-19.
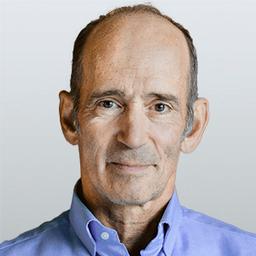
Dr. Joseph Mercola is the founder of Mercola.com. An osteopathic physician, best-selling author, and recipient of multiple awards in the field of natural health, his primary vision is to change the modern health paradigm by providing people with a valuable resource to help them take control of their health.
Author’s Selected Articles