A widely cited statistic that appears in several studies says that stress-related complaints are linked to 75 percent to 90 percent of doctor visits. Stress suppresses the immune system, causes the largest volume of lost work days, triggers episodes in diseases from asthma to gastrointestinal disorders, and is a major factor in top-killing diseases such as cancer and cardiovascular disease.
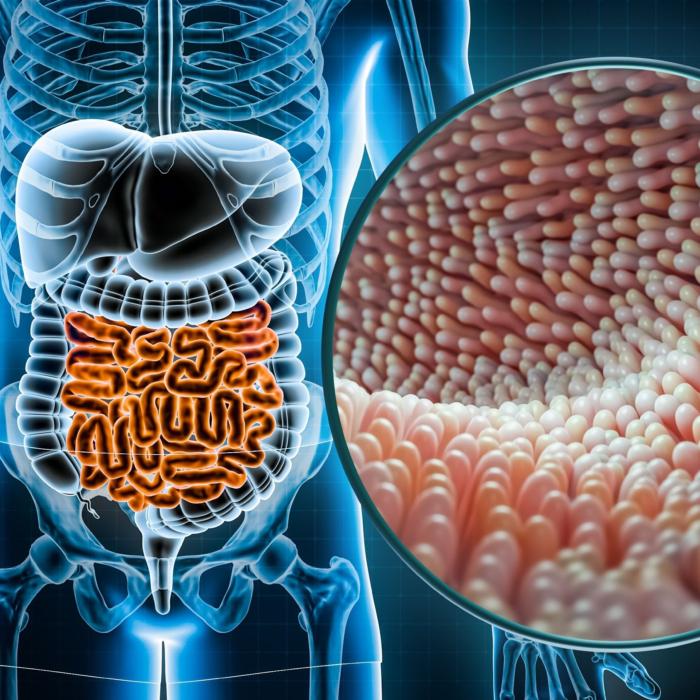
Stress appears to do this damage in part by influencing our gut microbiome. This symbiotic community of microbes that live inside us is made of trillions of bacteria, viruses, and fungi—and it’s very vulnerable to changes in its environment, the human body.