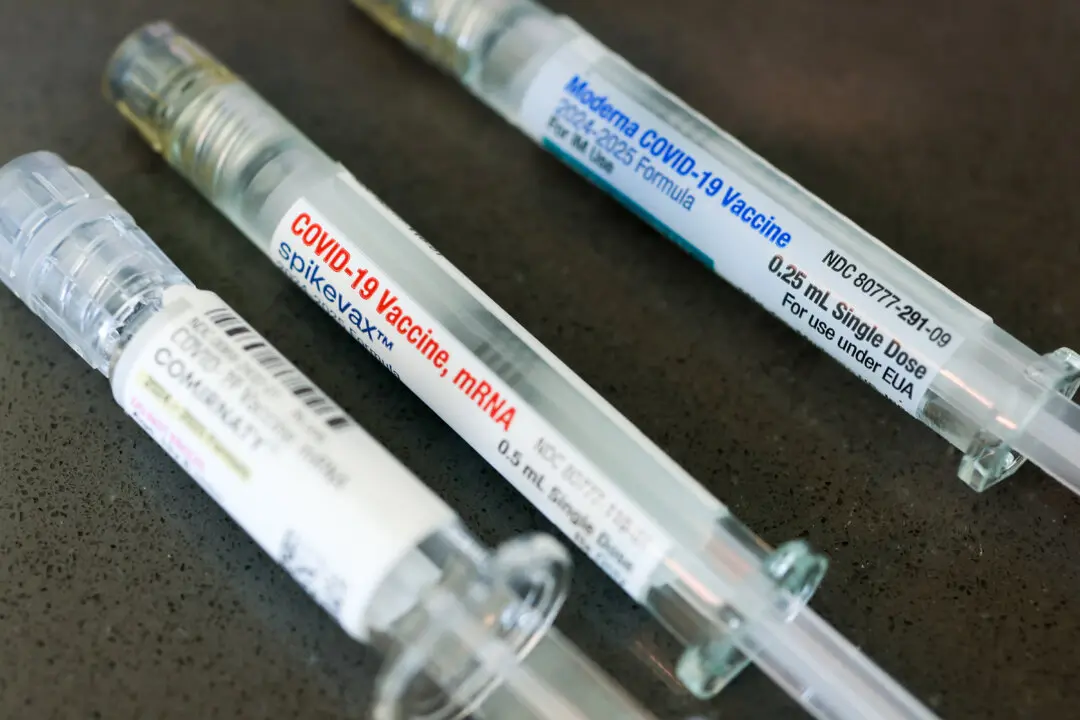
Numerous doctors treating long COVID and COVID-19 vaccine injuries now suggest fasting as a potential therapy for overall symptom improvement.
Before the COVID-19 pandemic, fasting was primarily used to treat metabolic diseases, with a number of doctors recommending it for weight loss and diabetes management. However, this therapeutic approach may also benefit individuals without these specific needs or ailments.