Dehydration from diarrhea, either from viral infection or cholera, accounts for 10 percent of all child deaths—a total of 700,000 children—worldwide each year.
Though it’s a pervasive problem, there are no clinical guidelines that perform better than chance for assessing dehydration severity. But now, researchers report that they statistically derived two simple diagnostic tools with high sensitivity and specificity from the cases of 771 children aged 0 to 5 in Dhaka, Bangladesh.
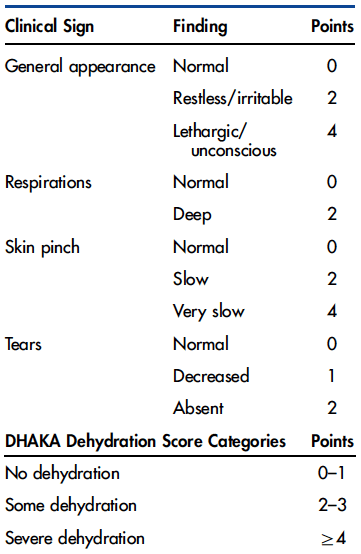
Named for the city where thousands of children suffer diarrhea-related dehydration every spring as cholera cases mount, the Dehydration: Assessing Kids Accurately (DHAKA) system includes both a simple scoring tool and a decision tree that clinicians can quickly apply when young patients arrive at a clinic.
Both tools require observing only a few symptoms that are readily apparent in a young child.