It has been known for some time that during pregnancy, the placenta enables a two-way trafficking of immune cells between mother and fetus. Some of the exchanged cells are capable of establishing long-lasting cell lines that persist for at least half a century after birth and are immunologically active.
Known as microchimerism, two genetically distinct and separately derived populations of cells are present in the same individual or organ. While it can occur artificially, as with recipients of blood transfusions or bone marrow transplants, it occurs naturally during most pregnancies. For instance, approximately 50-75% of women after giving birth carry fetal immune cells, and about half as many offspring carry maternal immune cells.
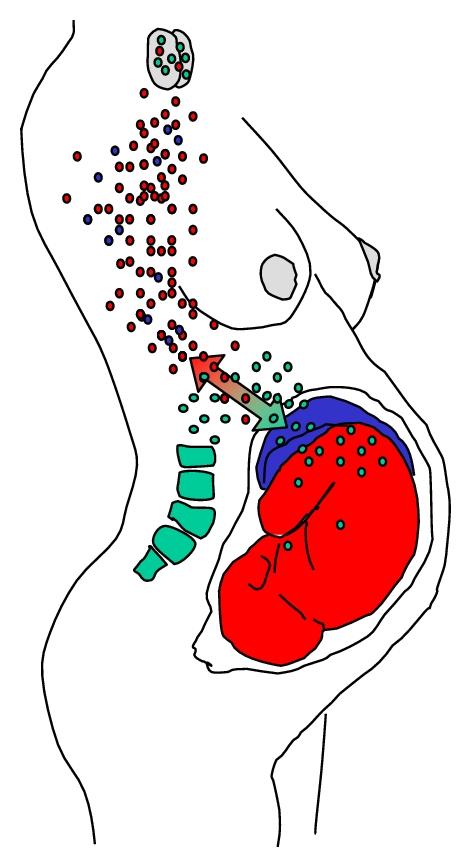
The bidirectional fetomaternal trafficking of cells through the placenta is known as “fetal microchimerism” when moving in the fetal -> maternal direction, and “maternal microchimerism” when moving in the maternal -> fetal direction.