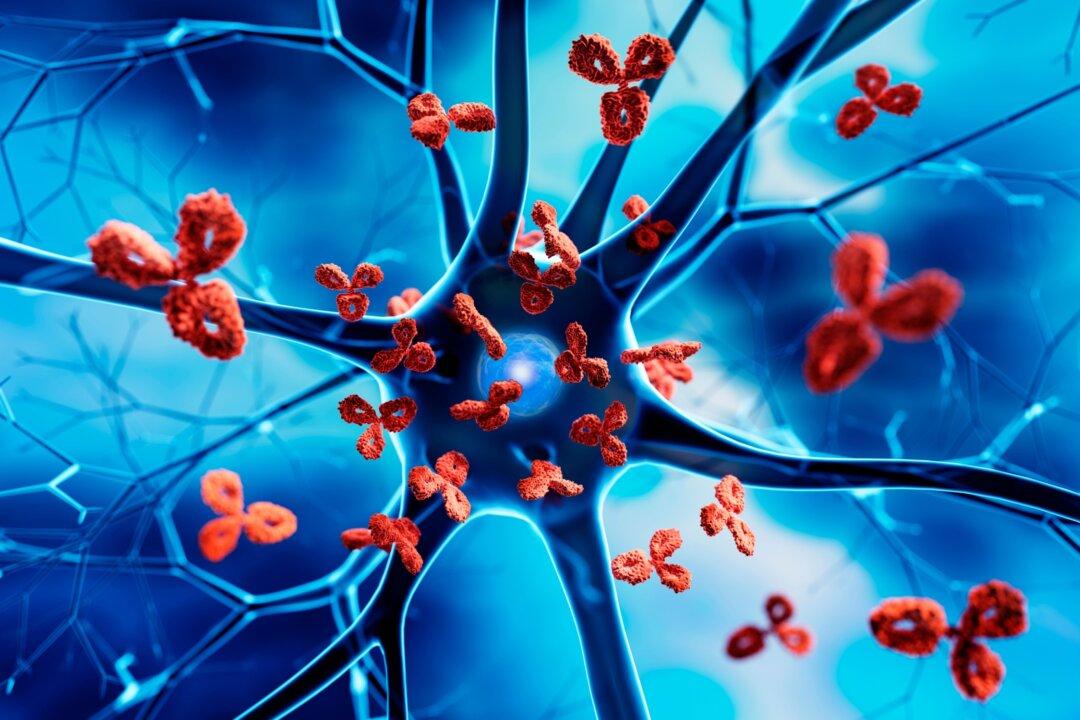
Do you or your patients ever suffer from brain fog, that feeling like you’re disconnected from the world, moving in a daze, and slow to process information? If so, take this symptom very seriously as it’s one of the earliest signs of neurodegeneration, or accelerated brain aging. This means you are at increased risk of Alzheimer’s, dementia, Parkinson’s, and other neurodegenerative diseases.
Brain fog is a symptom of an inflamed brain. The brain’s immune cells are called glial cells and they function and behave differently than immune cells in the rest of the body. When glial cells become activated, or primed, they become inflammatory. As they don’t have an automatic off switch, they can be inflammatory on an ongoing basis, damaging brain tissue in the process.