The National Institutes of Health (NIH) is conducting a multi-site clinical trial to evaluate Shionogi & Co.’s Xocova COVID-19 antiviral drug to determine its effectiveness in improving care for afflicted individuals.
“The study team will conduct analyses to understand any statistically significant differences—meaning those unlikely due to chance—between the treatment group and the placebo group. The key metric they will focus on is whether people receiving S-217622 recover (defined as returning home and remaining alive through day 60) more quickly than those in the placebo group.”
Results from a phase 3 trial that Shionogi conducted mainly in Japan had shown that the antiviral reduced COVID-19 symptoms among people with mild-to-moderate illness irrespective of vaccination status or risk factors.
Japanese Approval and Restrictions, NIH Study Procedure
Xocova was granted emergency regulatory approval in Japan in November 2022. Back in April 2022, the drug had come under scrutiny after preclinical studies had shown that it disturbed fetal development. As such, the Japanese approval excludes pregnant women from taking Xocova.Moreover, the medication cannot be used together with 36 other drugs, some of them taken for the treatment of hyperlipidemia and high blood pressure.
The NIH-funded study will involve participants being assigned to receive S-217622 or a placebo at random, with neither the participants nor investigators knowing who is receiving the drug. The medication will be taken once per day for five days.
Investigators will monitor and record the health status of participants for every day in the first week and then pre-specified days for the next 60 days. They will also collect nose swabs and blood samples of the participants for testing.
COVID-19 Antivirals and Potential Dangers
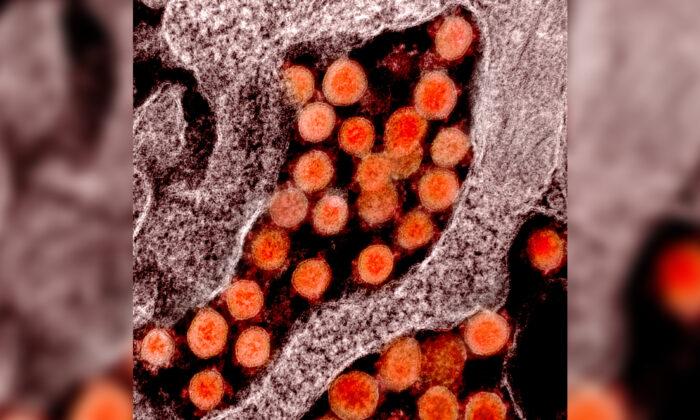
Xocova is an antiviral medication similar to Pfizer Inc.’s Paxlovid and Merck & Co. Inc.’s Lagevrio (molnupiravir) and is thus different from COVID-19 vaccines.The main difference between vaccinations and antivirals is that while a vaccine prevents a virus from invading a body by providing protection, antivirals seek to treat a virus that is already present in the body by delaying the infection.
Like Xocova, Lagevrio carries a warning that pregnant women should not consume the medication after animal studies found that it harmed fetuses. Even though Paxlovid was found to cause a decrease in fetal body weight at high doses in studies involving rabbits, no restrictions have been put on the drug’s use among pregnant women.
Paxlovid was approved for Emergency Use Authorization (EUA) in the United States in December 2021. In July 2022, the U.S. Food and Drug Administration allowed pharmacists to prescribe Paxlovid. However, this attracted concerns and disapproval from some clinicians because prescribing medications is primarily the responsibility of doctors.
Unlike pharmacists, physicians are well aware of a patient’s medical histories, allergies, intolerances, and other medications they take. As such, physicians can avoid prescribing medications with potential adverse effects that can come from drug interactions.
Paxlovid can interact with at least 43 different classes of drugs and more than 550 active drug ingredients, with some of these interactions potentially dangerous.