Early tests of radically redesigned antibiotics suggest the drugs could bolster defenses against biowarfare and bioterrorism.
In a study of animal cells and macrophages, researchers used two inhibitors—KKL-10 and KKL-40—to stop the proliferation of Franscisella tularensis, bacteria that the U.S. Centers for Disease Control classifies as a tier 1 select agent because the strain is highly infective and easily spread, says Kenneth Keiler, professor of biochemistry and molecular biology at Penn State.
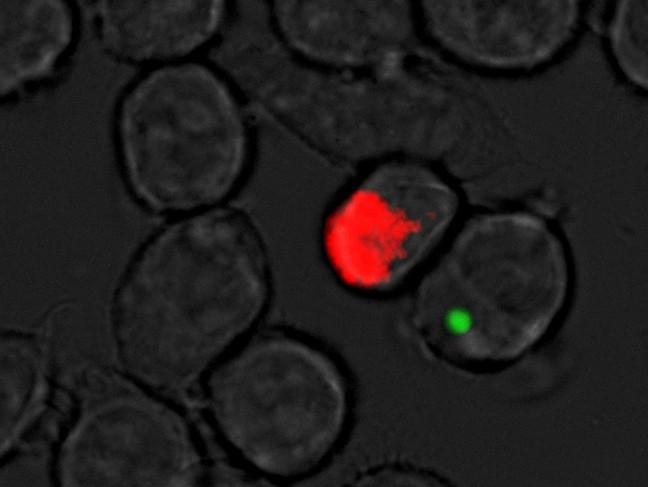
The new antibiotic compounds stopped Franscisella Tularensis, a virulent strain bacteria used in biowarfare, from spreading in animal cells. Girish Kirimanjeswara/Penn State




