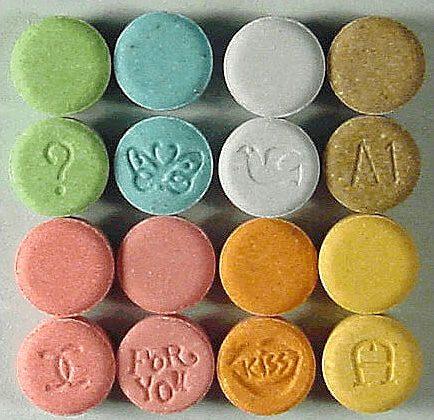
The approval of MDMA and “magic mushrooms” for certain medical conditions by the Therapeutic Goods Administration (TGA) has received a mixed response, with Australia’s peak psychiatric body saying further evidence is needed to determine the drugs’ long-term safety and efficacy.
According to the TGA, both drugs were reclassified from a schedule nine listing to a schedule eight listing, meaning they can be prescribed by authorised psychiatrists along with control measures. These control measures include having a human research ethics committee approve each case and using treatments alongside psychotherapy.
However, in its reclassification notice, the TGA admits that there are currently no established treatment protocols.
“My decision recognises that the evidence landscape is rapidly evolving toward establishing such protocols, and so places the onus and opportunity with a prospective prescriber of the Substances to devise and provide evidence of a suitable treatment protocol to the Human Research Ethics Committee (HREC) and authorising TGA officer,” a delegate of the Secretary of the Department of Health and Aged Care said.
Meanwhile, Professor Susan Rossell, a cognitive neuropsychologist and professorial research fellow at the Centre for Mental Health at Melbourne’s Swinburne University, is concerned the approval process has been rushed.
Ms. Rossell is conducting a phase 2 trial on the use of psilocybin-assisted psychotherapy in treatment-resistant depression.
Australian National University Associate Professor David Caldicott said the classification change represented an inevitable outcome that could have occurred in the 1980s.
“MDMA was being used as medication in 1985 when it was banned by executive order of the President of the USA, and against the advice of medical professionals and administrative agencies,” Mr. Caldicott said.
“Perhaps most excitingly, many of the treatments that are emerging with these previously banned products require only a brief exposure to facilitate therapy, and not the life-long prescription of drugs that do little more than dull the edge of psychological trauma.”
At the same time, Dr. Paul Liknaitzky from Monash University’s clinical psychedelic research project told SBS that psychedelic treatments have changed people’s lives.
“Yet the safety and effectiveness of psychedelic therapies depend on a unique set of professional competencies and considerations that are in scarce supply within mental healthcare,” Mr. Liknaitzky said.
Australia’s Peak Body Representing Psychiatrists Caught By Surprise
Richard Harvey, chair of the Psychedelic Assisted Therapy Steering Group at the Royal Australian and New Zealand College of Psychiatrists (RANZCP), said he was surprised by the TGA’s reclassification.“We have previously made submissions to the TGA, really not recommending that they do this. We just feel that the timing is, for a start, very, very short notice to introduce a completely new treatment paradigm that requires substantial resources and development,” Mr. Harvey told the BMJ.
Mr. Harvey added that treatment with MDMA or psilocybin should be administered as part of an intensive psychotherapy program with two trained psychiatrists for 40 hours.
Martin Williams, a mental health researcher from the Centre for Mental Health at Swinburne University, said the studies so far had been conducted in small, carefully chosen patient populations that excluded people with other conditions such as personality disorders or substance use disorders.
Psychedelic-Assisted Therapies Still in Infancy
In an op-ed, psychiatrist and clinical associate at The Centre of Mental Health, Nigel Strauss, said that despite a growing body of evidence that supports the use of psychedelics for PTSD and depression, the use of these drugs is still in its infancy.“Psychedelic-assisted therapy is no miracle cure. Espousing the benefits without a thorough examination of the risks and limitations is not only a misrepresentation of the science, it is arguably unethical.
“There is potential for psychedelic substances to cause fear, panic or cause psychological damage if given to susceptible and vulnerable people who have been inadequately screened or assessed.
“Paranoia, traumatisation, worsening depression, and even suicidal behaviour, among other serious side-effects, have been observed in some cases.”
Swinburne University in Melbourne, Australia, signed a $5 million (US$3.46 million) clinical research agreement with Woke Pharmaceuticals to examine the effects of psilocybin—the active ingredient in psychedelic mushrooms—in treating treatment-resistant depression.