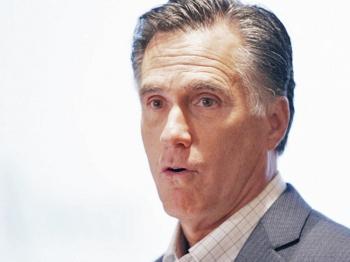
BOSTON—Massachusetts became the first state to implement universal health coverage five years ago. Its plan, developed under then-Gov. Mitt Romney, paved the way for the 2010 federal health care overhaul. Gov. Deval Patrick announced that now more than 98 percent of residents are covered, and that the plan reduced state costs.
The 2006 legislation required nearly all Massachusetts residents to sign up for health care insurance or face tax penalties. For the low-income uninsured, it provided subsidized low-or no-cost health insurance to those who qualify through Commonwealth Care—a state-regulated minimum level of health care insurance coverage.
In recent official statements, Patrick outlined the successes of the health care reform effort and announced that the state is expected to save of $80 million on Commonwealth Care in 2012, which allows state funding to remain level, even as enrollment is projected to grow by 11 percent. The state gave Commonwealth Care $822 million for fiscal year 2011, and 158,000 residents are enrolled in it.
According to the administration, in fiscal year 2012, enrollment is expected to grow to 175,000. Copayments will not go up. Premiums for the lowest-cost plans are expected to stay at 2008 levels.
“Today, thanks to effective implementation of our 2006 reform legislation, we lead the nation in providing health care to our residents,” stated Patrick in a press release. “More than 98 percent of Massachusetts residents have health care coverage, including 99.8 percent of our children.”
“Now, just as we have provided the national model for universal access, I believe we can crack the code on cost control,” said Patrick.
According to recent releases, Massachusetts paid over $700 million in 2005 for health care for the uninsured and underinsured. In fiscal year 2011, it spent about $400 million—nearly $300 million less.
The percentage of private companies offering health insurance to their employees has grown to 77 percent from 70 percent before the bill was passed. That compares to 69 percent nationwide.
Health care reform in Massachusetts has not been a budget buster. Universal coverage has added only about 1 percent more of our state budget in state spending.
As of June 2010, more than 400,000 people in Massachusetts had insurance than had previously been uninsured.
The Commonwealth Care program has achieved $80 million in cost savings for next year by encouraging competition and innovation among health plans, the state reported. A number of the managed care organizations that provide coverage in the program submitted bids for next year at significantly lower rates than their current rates, resulting in the savings.
Gov. Deval Patrick said the lower rates were achieved through renegotiated provider contracts, narrower choices of hospitals, doctors and specialists, and new medical management programs.
“The state’s new fiscal reality demands that we change the way government does business to stretch every taxpayer dollar as far as possible to preserve critical programs and services,” said Secretary of Administration and Finance Jay Gonzalez, who also chairs the Health Connector (Commonwealth Care) board of directors.
The $80 million projected savings are only a preliminary effort at health cost containment though it should win support for Patrick’s next phase of comprehensive payment reform.
The 2009 fiscal report on the Implementation of Health Care Reform proposed moving from a predominantly fee-for-service based system to a global payment based system. That means giving a lump sum payment to new networks called accountable care organizations (ACOs) that consists of doctors, hospitals, home care providers, and mental health and rehab centers that will be responsible for the patients assigned to them.
The providers will have discretion to manage the best care they can provide using the most cost effective measures available. If a team can provide care for less, they can keep some of the savings based on a prescribed set of rules. Arguments for it say that it provides incentive for preventive care, and removes incentives for unneeded procedures. Arguments against it say that doctors could suffer financial losses by taking on patients with costly, chronic illnesses such as diabetes.
The first cost-containment debate in the Legislature is scheduled for May 16.
The 2006 legislation required nearly all Massachusetts residents to sign up for health care insurance or face tax penalties. For the low-income uninsured, it provided subsidized low-or no-cost health insurance to those who qualify through Commonwealth Care—a state-regulated minimum level of health care insurance coverage.
In recent official statements, Patrick outlined the successes of the health care reform effort and announced that the state is expected to save of $80 million on Commonwealth Care in 2012, which allows state funding to remain level, even as enrollment is projected to grow by 11 percent. The state gave Commonwealth Care $822 million for fiscal year 2011, and 158,000 residents are enrolled in it.
According to the administration, in fiscal year 2012, enrollment is expected to grow to 175,000. Copayments will not go up. Premiums for the lowest-cost plans are expected to stay at 2008 levels.
“Today, thanks to effective implementation of our 2006 reform legislation, we lead the nation in providing health care to our residents,” stated Patrick in a press release. “More than 98 percent of Massachusetts residents have health care coverage, including 99.8 percent of our children.”
“Now, just as we have provided the national model for universal access, I believe we can crack the code on cost control,” said Patrick.
According to recent releases, Massachusetts paid over $700 million in 2005 for health care for the uninsured and underinsured. In fiscal year 2011, it spent about $400 million—nearly $300 million less.
The percentage of private companies offering health insurance to their employees has grown to 77 percent from 70 percent before the bill was passed. That compares to 69 percent nationwide.
Health care reform in Massachusetts has not been a budget buster. Universal coverage has added only about 1 percent more of our state budget in state spending.
As of June 2010, more than 400,000 people in Massachusetts had insurance than had previously been uninsured.
The Commonwealth Care program has achieved $80 million in cost savings for next year by encouraging competition and innovation among health plans, the state reported. A number of the managed care organizations that provide coverage in the program submitted bids for next year at significantly lower rates than their current rates, resulting in the savings.
Gov. Deval Patrick said the lower rates were achieved through renegotiated provider contracts, narrower choices of hospitals, doctors and specialists, and new medical management programs.
“The state’s new fiscal reality demands that we change the way government does business to stretch every taxpayer dollar as far as possible to preserve critical programs and services,” said Secretary of Administration and Finance Jay Gonzalez, who also chairs the Health Connector (Commonwealth Care) board of directors.
The $80 million projected savings are only a preliminary effort at health cost containment though it should win support for Patrick’s next phase of comprehensive payment reform.
The 2009 fiscal report on the Implementation of Health Care Reform proposed moving from a predominantly fee-for-service based system to a global payment based system. That means giving a lump sum payment to new networks called accountable care organizations (ACOs) that consists of doctors, hospitals, home care providers, and mental health and rehab centers that will be responsible for the patients assigned to them.
The providers will have discretion to manage the best care they can provide using the most cost effective measures available. If a team can provide care for less, they can keep some of the savings based on a prescribed set of rules. Arguments for it say that it provides incentive for preventive care, and removes incentives for unneeded procedures. Arguments against it say that doctors could suffer financial losses by taking on patients with costly, chronic illnesses such as diabetes.
The first cost-containment debate in the Legislature is scheduled for May 16.