SPECIAL COVERAGE
Read More
Read More
‘Explosions’ Heard in Iran, Flights Divert
This unfolds against the backdrop of heightened tensions following Iran’s unprecedented missile-and-drone attack on Israel on April 13.
‘Explosions’ Heard in Iran, Flights Divert
This unfolds against the backdrop of heightened tensions following Iran’s unprecedented missile-and-drone attack on Israel on April 13.
Trending Videos
Top Premium Reads
Top Stories
Most Read
Foreign Aid Package For Ukraine, Israel Advances to House Floor
Democrats stepped in to help advance the bills to floor to overcome three conservatives who voted against it.
Proposal to Reform California’s Prop. 47 Gets Enough Signatures to Appear on Ballot
Supporters collected more than 900,000 signatures to place the tough-on-crime measure on the November ballot.
Congressman Introduces Bill to Stop Cobalt Mined by Child Exploitation and Forced Labor From Entering US Market
Cobalt is a key natural resource used to power electric vehicles, solar panels, and other purportedly “green” products. Around 90 percent of it originates from
FBI Warns Chinese Hackers Are Poised to Hit US Infrastructure Anytime With ‘Devastating Blow’
‘Its plan is to land low blows against civilian infrastructure to try to induce panic,’ FBI Director Christopher Wray said.
Gaetz Raises Alarm Over Lockheed Martin’s Control of F-35 Fighter Jet Program
As of February 2023, only 29 percent of the United States’ F-35 jets were considered ‘fully mission capable.’
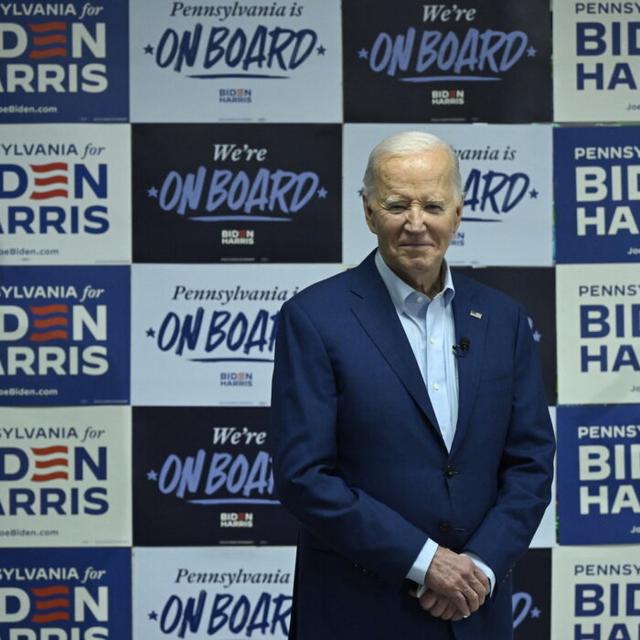
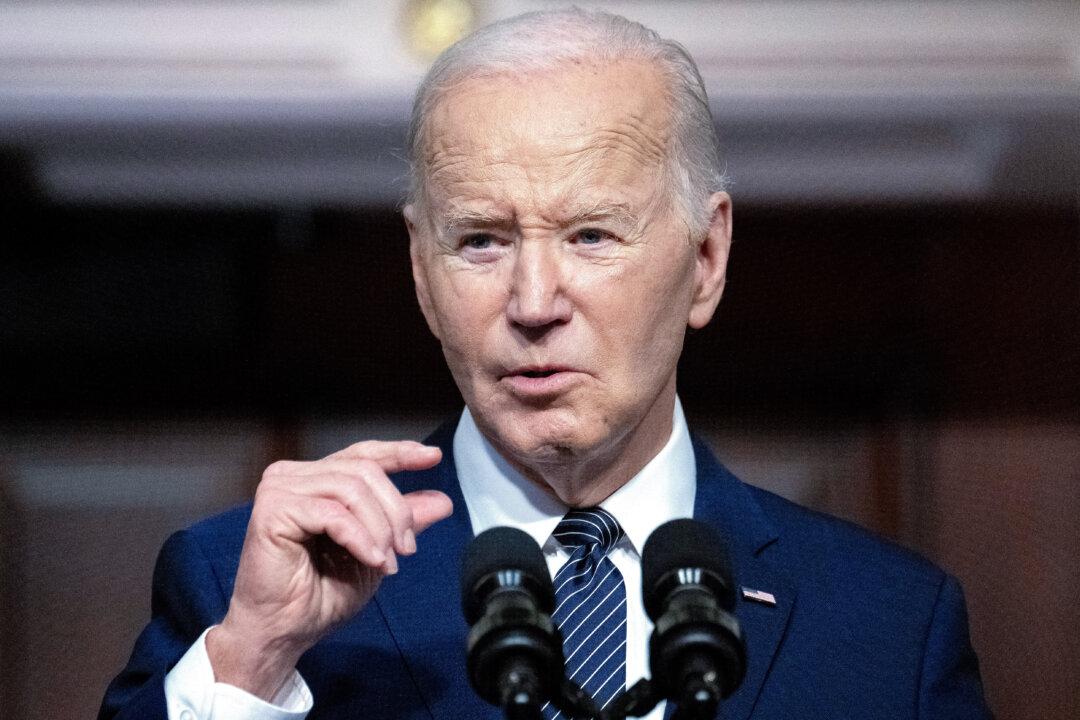
Biden Calls Beijing ‘Xenophobic,’ Says the Regime Is ‘Cheating’ America on Trade
‘They’re xenophobic—nobody else coming in. They’ve got real problems.’
Amid Budget Shortfall, San Francisco Reexamines Tax Burden on Big Businesses
City leaders are negotiating with business execs and labor to craft reforms that would simplify taxes.
Chinese Embassy’s Reported TikTok Lobbying Triggers Bipartisan Outrage
Lawmakers say that the Chinese embassy’s moves show that the CCP considers TikTok a ’strategic asset' for influence operations in America.
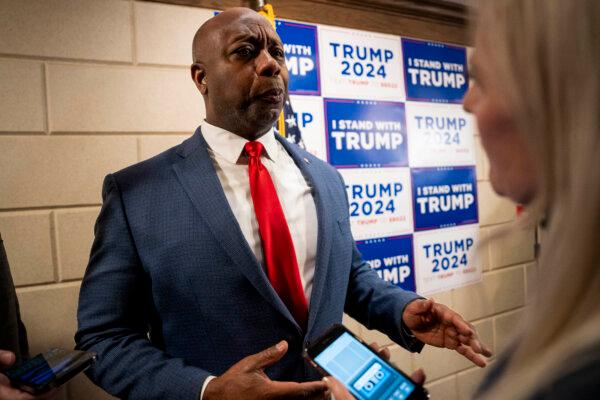
Trump New York Trial Makes Headway as Full Jury Seated
Opening statements are scheduled for April 22, and court will adjourn at 2 p.m. to accommodate those who need to leave for Passover.
Top Military Official Lied About Jan. 6: Whistleblowers
Army Secretary Ryan McCarthy was among senior officials who did not tell the truth about what happened on Jan. 6, 2021, National Guard officials say.
Johnson Says He Won’t Change Motion to Vacate Rule After Republican Pushback
House Speaker Mike Johnson (R-La.) was openly critical of the motion to vacate but announced that he wouldn’t be pursuing a rule change.
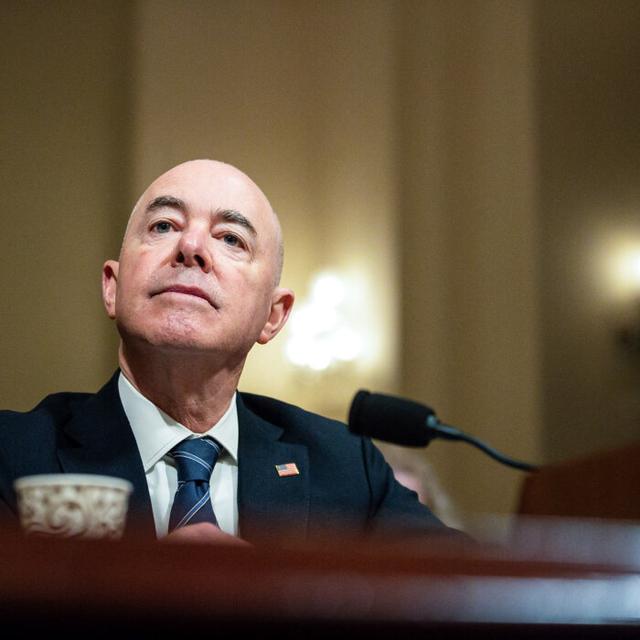
National Security Concerns Raised as Number of Chinese Military-Age Illegal Immigrants Hits Record High
‘Illegal border crossings by Chinese nationals are skyrocketing,’ said Florida Rep. Brian Mast. ‘This is a national security threat.’
Texas Is Enforcing Federal Immigration Laws: Gov. DeSantis
Instead of executing laws to check illegal immigration, the federal government is ‘intentionally violating’ them.

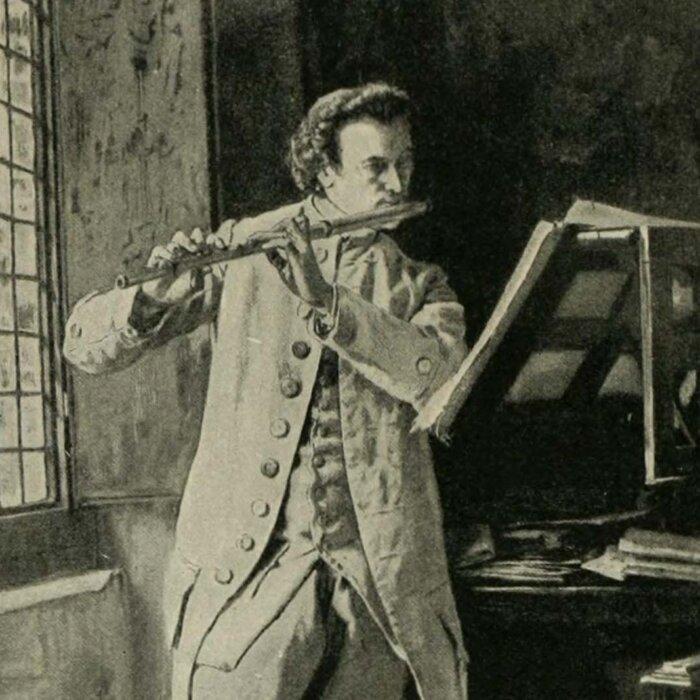
The American Mozart: Composer Timothy Olmsted
Timothy Olmsted’s lifelong dedication to music made him one of the country’s earliest influential musicians.
The American Mozart: Composer Timothy Olmsted
Timothy Olmsted’s lifelong dedication to music made him one of the country’s earliest influential musicians.
Epoch Readers’ Stories
Wisdom From a Retired Cowboy Artist
I have lived the life of the sculptures I have made.
Section 3 of 14th Amendment Not Applicable for Ruling Trump out of 2024
I don’t believe that Section 3 of 14th Amendment is self-executive and therefore can not be applied directly by the court.
Inspired Stories
Empower the World with Your Story: Share Love, Inspiration, and Hope with Millions
Special Coverage
Special Coverage
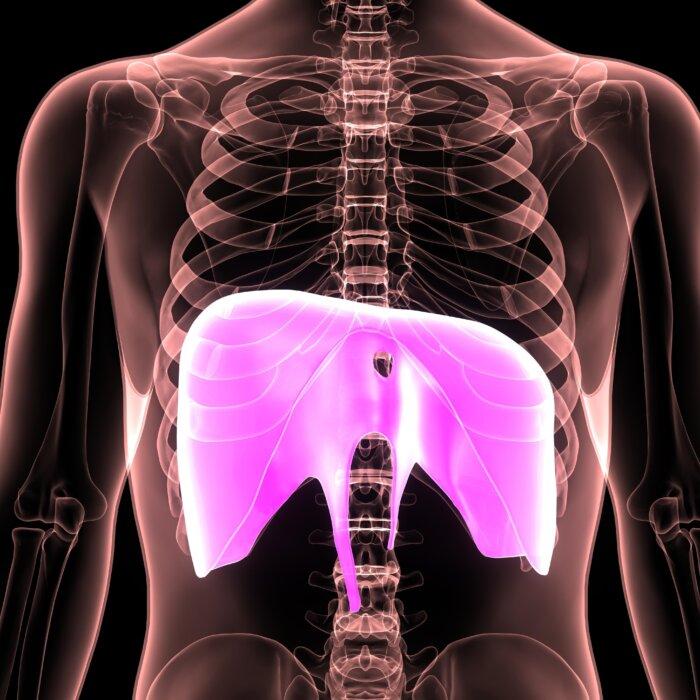
Study Finds ‘Significant Increase’ in Cancer Mortality After Mass Vaccination With 3rd COVID Dose
Numerous mechanisms may explain how mRNA COVID-19 vaccines may be linked to increased cancer deaths.
Study Finds ‘Significant Increase’ in Cancer Mortality After Mass Vaccination With 3rd COVID Dose
Numerous mechanisms may explain how mRNA COVID-19 vaccines may be linked to increased cancer deaths.

‘Hart’s War’: Soldiers Shaping War and Being Shaped by It
A court-martial at the POW camp is not what it seems to be in this film by director Gregory Hoblit.

‘Monsieur Chopin: A Play With Music’
This one-man play celebrates the life and music of one great composer.

S. Truett Cathy: Founder of Chick-fil-A
This entrepreneur called on his ethic of hard work to build a successful fast food franchise.

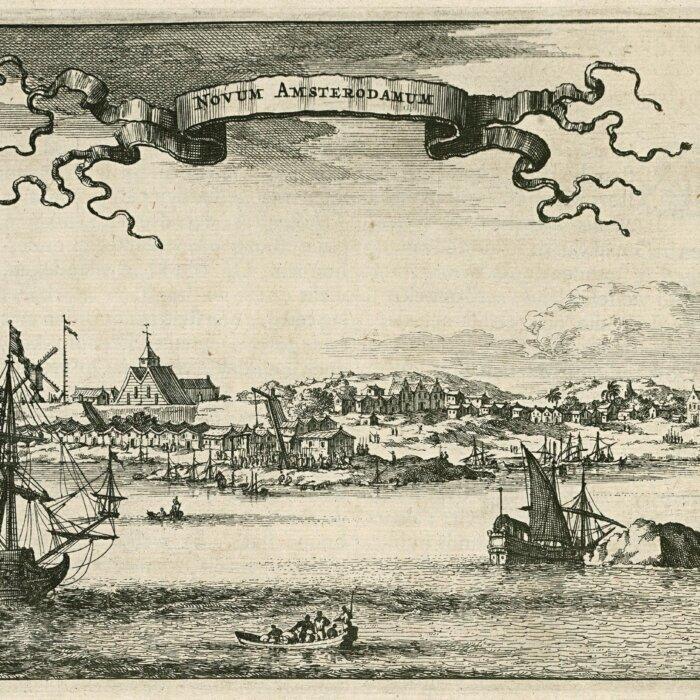
Rembrandt’s Sole Seascape and the Great Heist
Stolen from the Isabella Stewart Gardner Museum in 1990, ‘Christ in the Storm on the Sea of Galilee’ along with two other Rembrandts are still missing.

Where Time Stands Still: Mast General Store
The general stores encapsulates a bygone era for travelers in North Carolina.

Best Meatloaf Recipe (Tender & Juicy)
This Best Meatloaf Recipe is packed with flavor and tenderness. The secret is the tangy and savory sauce added to the meatloaf as it bakes.
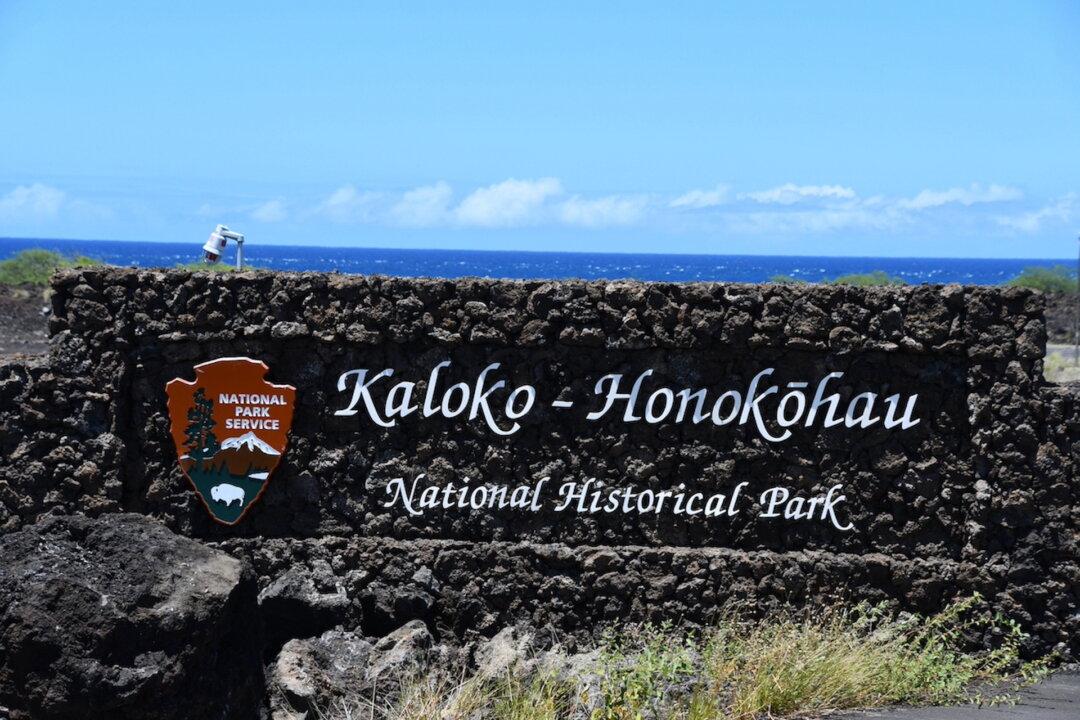
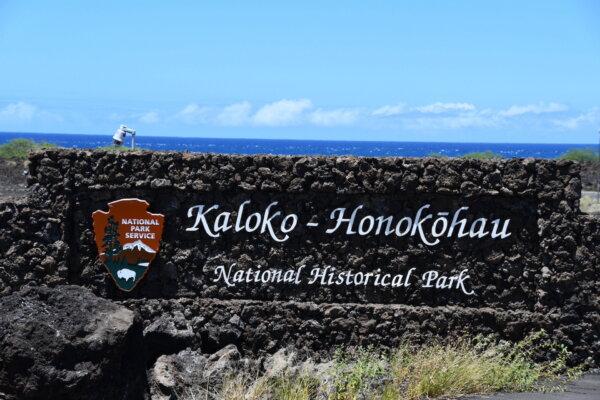
Taking the Kids: And Heading to Less Visited National Parks
There are 429 national park sites in the U.S., though just 63 have the “National Park” designation in their names.

Thailand Leads Push for Six-Nation Visa to Lure Moneyed Tourists
The plan is so that tourists can travel six countries on one visa, but some officials are not optimistic.

Brazil Postpones Visa Requirements Once Again for American Visitors
The goal is to ensure that Brazil’s electronic visa program is fully up and running before applying the visa requirement.
Taking the Kids: And Heading to Less Visited National Parks
There are 429 national park sites in the U.S., though just 63 have the “National Park” designation in their names.












![[LIVE on 4.19 1PM ET] How Diet, Lifestyle Could End 80 Percent of Diabetes, Cancer, Other Disease](/_next/image?url=https%3A%2F%2Fimg.theepochtimes.com%2Fassets%2Fuploads%2F2024%2F04%2F13%2Fid5628731-Food-Matters-web-1920x1080-1.jpeg&w=1200&q=75)
![[LIVE on 4.19 1PM ET] How Diet, Lifestyle Could End 80 Percent of Diabetes, Cancer, Other Disease](/_next/image?url=https%3A%2F%2Fimg.theepochtimes.com%2Fassets%2Fuploads%2F2024%2F04%2F13%2Fid5628731-Food-Matters-web-1920x1080-1-1080x720.jpeg&w=1200&q=75)


































































































![[LIVE Q&A 04/19 at 10:30AM ET] Major Case Could Overturn Jan. 6 Charges](/_next/image?url=https%3A%2F%2Fimg.theepochtimes.com%2Fassets%2Fuploads%2F2024%2F04%2F18%2Fid5632533-CR-TN_REC_0419-600x338.jpg&w=1200&q=75)